The recent statement issued by the Nigerian Association of Resident Doctors (NARD), objecting to the proposed upgrade of academic titles for Pharmacy, Physiotherapy, and Optometry programs, has reignited an old debate that continues to impede meaningful progress in Nigeria’s healthcare system. This opposition, rather than safeguarding standards, reflects a deep-seated professional insecurity and a reluctance to embrace global best practices that prioritize patient-centered, collaborative care.
At the core of NARD’s resistance is a misplaced concern that advancing the academic standing and clinical roles of other healthcare professionals somehow diminishes the authority or relevance of medical doctors. This view is both antiquated and counterproductive. The modernization of degree nomenclature by the National Universities Commission (NUC) is not an attempt to rival or undermine the medical profession; rather, it is a recognition that academic rigor and clinical competence are not the exclusive preserve of physicians.
Around the world, healthcare has evolved into a system where interdisciplinary collaboration is not only encouraged but essential for optimal patient outcomes. Nigeria’s healthcare landscape should be no different. Several global examples illustrate how healthcare professions have advanced harmoniously without the internecine conflicts that seem to persist here:
United States: The Doctor of Physical Therapy (DPT) has been the entry-level qualification since 2016. Physical therapists have direct access rights, meaning patients can consult them without a physician referral. They independently evaluate, diagnose within scope, and manage patients — all in collaboration with other healthcare providers.
Canada: Physiotherapists routinely work with advanced clinical responsibilities, including direct access to patients. Master’s and Doctorate-level qualifications are standard, and interdisciplinary cooperation is embedded within healthcare delivery.
Australia: Physiotherapists can independently order diagnostic imaging, prescribe certain medications, and manage complex conditions. Many hold doctoral degrees and work closely with physicians and other healthcare professionals in integrated settings.
United Kingdom: Advanced practice physiotherapists prescribe medications, order imaging, and perform injections independently. The use of the title “Doctor” is regulated but appropriately extended to qualified non-physician healthcare professionals without controversy.
Western Europe: Countries like the Netherlands, Norway, and Belgium have empowered physiotherapists with direct access and advanced clinical rights, underpinned by doctoral-level education. These healthcare systems function efficiently without professional turf wars.
These examples demonstrate that empowering all healthcare professions to practice at the top of their scope improves access, efficiency, and patient outcomes. Rather than fragmenting care, it strengthens the system.
The notion that only medical doctors should control or dictate the professional trajectory of other healthcare providers stems from a dated, hierarchical model of care. Modern healthcare requires interdependence, mutual respect, and recognition that no single profession holds a monopoly on knowledge or competence. Patients benefit most when healthcare teams operate as collaborative units, not as feudal kingdoms with rigid hierarchies.
Furthermore, the belief that professional titles alone equate to clinical supremacy is misguided. Competence is demonstrated through education, continuous professional development, and, most importantly, patient outcomes — not through the policing of nomenclature.
The NUC’s decision to modernize the academic titles of Pharmacy, Physiotherapy, and Optometry programs aligns Nigeria with international standards and acknowledges the evolving roles these professions play in delivering quality healthcare. Instead of resisting such reforms, all stakeholders — including NARD — should focus on how best to integrate these advancements for the benefit of Nigerian patients.
Ultimately, the strength of any healthcare system lies in its ability to harness the collective expertise of its professionals, each contributing uniquely within their scope. Territorialism serves no one — least of all the patients we are all sworn to serve.
It is time for Nigerian healthcare professionals to transcend outdated rivalries and embrace a model of care where collaboration, not competition, drives progress.
—
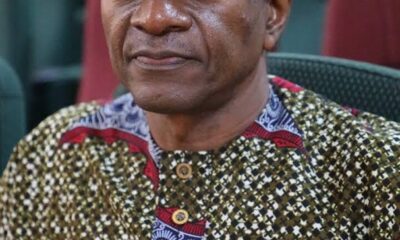
About the author
Dr. Abiodun A. Adeogun, PT, DPT, MSPT, is an experienced physical therapist, educator, and advocate with over 14 years of clinical practice in musculoskeletal, neurological, and cardiopulmonary rehabilitation. Having led multidisciplinary teams in both Nigeria and the United States, he is committed to advancing patient-centered care and mentoring the next generation of healthcare professionals. His published research emphasizes innovative rehabilitation strategies and the importance of accessible, evidence-based care for diverse patient populations. Dr. Adeogun remains a passionate voice for healthcare reform and professional development within the Nigerian and global healthcare communities.